Although the MBS item numbers for nicotine and smoking cessation counselling were only funded for a short time, there was strong demand for the session across the country.
“This is the way the MBS funding for tobacco cessation counselling ends, not with a whimper but a bang” – a poor man’s T.S. Eliot
Roughly 18 months have passed since the funding for Medicare Benefits Schedule item numbers relating to face-to-face and telehealth consults for nicotine and smoking cessation counselling provided by GPs and other medical practitioners ceased, but new data provided by Services Australia suggests there was a 16-fold increase in demand to access this support while the funding was available.
“Embedding smoking and nicotine cessation in routine care is essential, and the present study identified that claims processed for face-to-face services (which could be provided by a patient’s usual practice) increased from a rate of 1 to 16 per 1000 people who smoke between 2021 and 2023,” the researchers wrote in the Australian Journal of General Practice.
“The monitoring and evaluation of smoking and nicotine cessation as part of routine care are required to help ensure that appropriate supports and ongoing culturally safe best practice are implemented and maintained.”
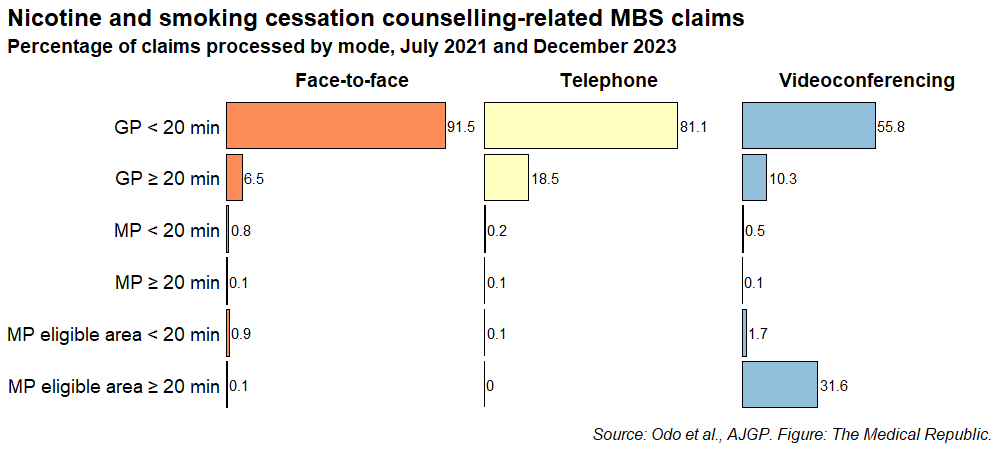
Researchers examined Medicare claims data for the 18 item numbers relating to smoking and nicotine cessation counselling for claims processed between July 2021 and December 2023.
There were 188,904 claims processed during this window, with nearly three quarters of these (139,667) offered in a face-to-face setting. The number of claims for telephone (37,649; 19.9%) and videoconferencing consults (11,588; 6.1%) were much smaller in comparison.
The majority of counselling sessions involved seeing a GP for less than 20 minutes, regardless of whether the session was face-to-face, via telephone or a videoconference. However, there was a higher level of demand for video-based counselling sessions with a medical practitioner in an eligible area that lasted for at least 20 minutes.
There was a 16-fold increase in the rate of face-to-face claims processed between July 2021 and December 2023, from 1 to 16 per 1000 people who smoke, with the extent to which the rate increased accelerating over time. There was also an increase in the rate of claims processed for telephone services during the same time period (from 0 to 2 per 1000 smokers), but the claim rate for videoconferencing remained steady over time.
The increase in demand for face-to-face counselling sessions was similar in men (0.7 to 15.3 per 1000 smokers) and women (0.7 to 16.6 per 1000), as was the increase for telephone-based sessions (0.2 to 2.0 per 1000 for men, 0.2 to 2.8 per 1000 for women).
Related
Lead author Dr Daniel Bogale Odo (PhD) said the withdrawal of funding for the range of Medicare item numbers was due to an assumption that the kind of counselling offered in these sessions had become, or was already, part of routine practice. However, there is a major – yet completely unexpected – barrier as to why the cessation counselling sessions had not become a part of regular practice.
“One of the frequently reported barriers to providing nicotine and smoking cessation support in clinical settings is a lack of time. The increase in the use of these temporarily funded Medicare items could be due to the allocation of adequate time and payment to provide this care,” the epidemiologist from the Australian National University told media.
“The cessation of these services might have had a regressive impact on people who want to quit seeking support from their GP at a time when many changes were occurring in respect of nicotine and tobacco control measures.”
Dr Michael Wright, president of the Royal Australian College of GPs, said smoking cessation needed to remain an urgent priority for the health of the nation.
“Almost 9000 people still die of lung cancer in Australia each year, and it is still our most common cancer death. Most of these deaths are preventable,” he said in a statement.
“GPs have a critical role to play in helping people to stop smoking and vaping. This study shows the difference embedding smoking and vaping cessation in routine care makes in people’s lives.”
Dr Wright was also keen to see a system that allowed patients to have affordable, longer consultations with their GPs on other health-related issues they may be experiencing.
“Smoking cessation is only one area where patients may need longer consults with their GP. Australia should have a health system that supports our patients to access affordable long consults with their GP when they need them.”