Adding CT scans and symptoms to spirometry improves diagnosis and identifies high-risk patients more accurately, researchers say.
A new diagnostic approach to chronic obstructive pulmonary disease that incorporates chest computed tomography findings and respiratory symptoms in addition to spirometry has been shown to improve the identification of individuals at high risk for adverse respiratory outcomes.
Findings from a large multicentre cohort study, published last month in JAMA, support a shift toward a more multidimensional definition of COPD.
The study analysed data from 9416 participants in the US-based COPDGene cohort and 1341 participants in the Canadian CanCOLD cohort.
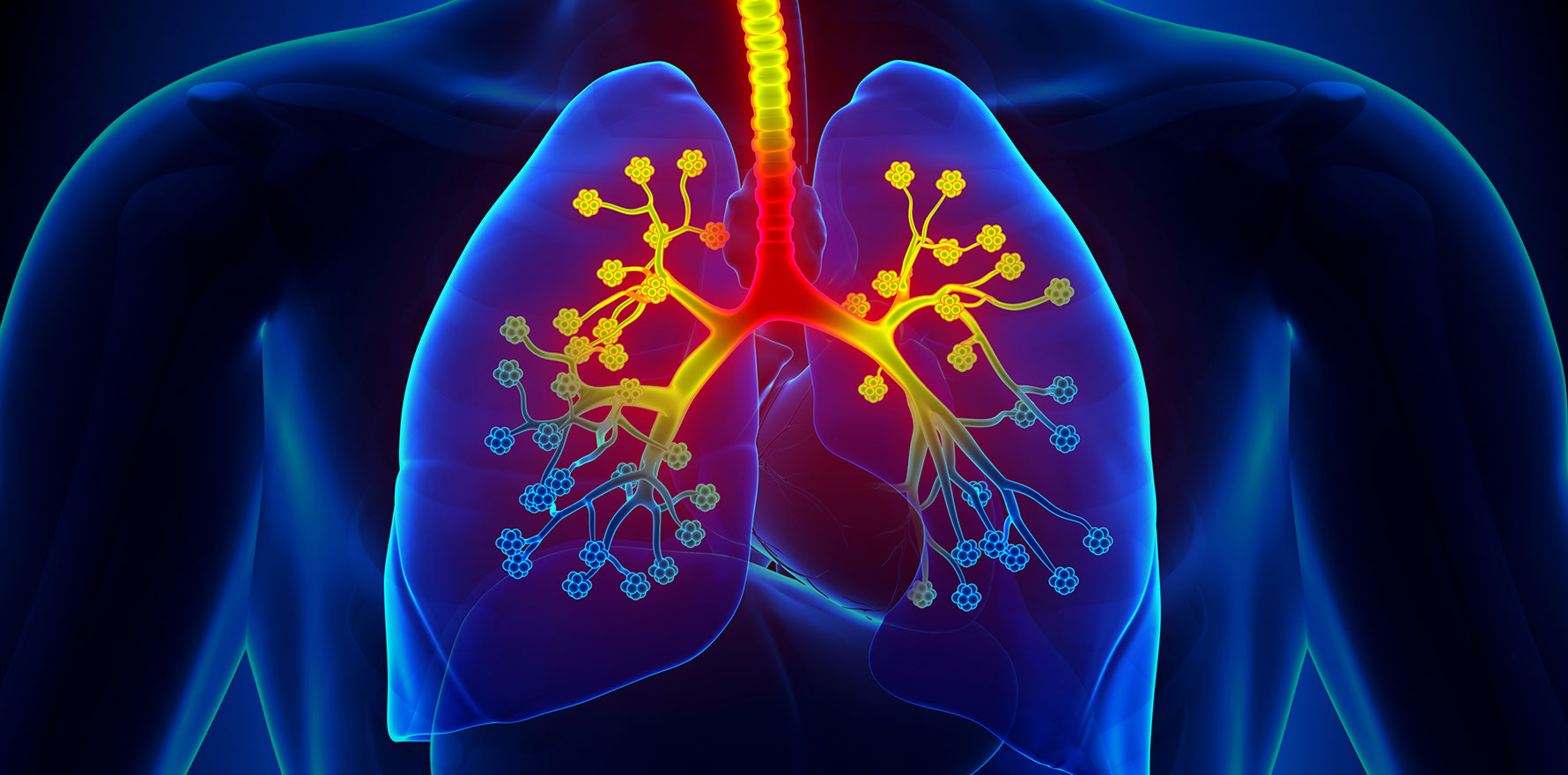
Researchers evaluated the utility of a novel diagnostic schema that includes not only traditional spirometry criteria (post-bronchodilator FEV₁/FVC <0.70), but also CT imaging abnormalities (emphysema or bronchial wall thickening), respiratory symptoms (e.g., dyspnoea, chronic bronchitis) and poor respiratory quality of life.
Participants were classified into two categories, including:
- Major diagnostic category: Presence of airflow obstruction plus at least one minor criterion (e.g., imaging abnormalities, symptoms).
- Minor diagnostic category: Absence of airflow obstruction but with ≥3 minor criteria, including both imaging abnormalities and symptoms.
International guidelines currently define COPD based on airflow obstruction measured by spirometry, specifically a post-bronchodilator FEV₁/FVC ratio <0.70 or below the lower limit of normal in the presence of respiratory symptoms. This approach has been the standard for decades.
However, the researchers said recent evidence showed that spirometry was not sensitive enough to detect early or structural lung changes associated with COPD. Many individuals — particularly long-term smokers — have abnormal chest CT findings such as emphysema or airway wall thickening without meeting spirometric criteria for COPD.
“Several studies have demonstrated that spirometry is not sensitive to the structural changes associated with COPD, which often occur before lung function decreases below the thresholds recommended for defining airflow obstruction,” the authors wrote. “Up to half of individuals with a history of cigarette smoking have evidence of emphysema or airway wall thickening on chest computed tomography (CT).
“Among individuals without airflow obstruction, the risk of developing it on spirometry within 5 years is 2-fold higher for those with airway wall thickening and 4-fold greater for those with emphysematous changes on chest CT compared with those who do not have structural abnormalities on chest CT.
Related
“Furthermore, 50% of individuals who currently smoke or formerly smoked and are without airflow obstruction have substantial respiratory symptoms, which may be attributed to aging, weight gain, deconditioning and smoking-induced cough, and these symptoms often are unreported.”
Because COPD is heterogeneous and multifactorial, relying solely on spirometry misses many patients with early or non-classic disease, the authors wrote.
In recognition of this, several efforts have been made to update diagnostic approaches, including the COPDGene 2019 criteria that introduced a four-part diagnostic model based on risk factors, symptoms, imaging findings and spirometry — requiring all four for a definite diagnosis. This led to some patients being excluded who might still be at risk, the authors wrote.
The 2022 Lancet Commission emphasised the need for a multidimensional diagnosis but did not specify exact thresholds, while the GOLD 2023 guidelines acknowledged that emphysema and airway abnormalities should raise suspicion for COPD, but did not formally incorporate imaging into the diagnostic algorithm.
The latest JAMA study set out to evaluate whether a new, expanded diagnostic schema that integrates respiratory symptoms, CT imaging, and spirometry, could more accurately identify patients at risk for mortality (all-cause and respiratory-specific), frequent exacerbations, and faster decline in lung function.
In the COPDGene cohort of 9416 adults, 15.4% of those without airflow obstruction were newly diagnosed with COPD under the new schema. These individuals had nearly double the risk of all-cause death, more than triple the risk of respiratory death, twice the rate of exacerbations and faster lung function decline compared with those not diagnosed with COPD.
Conversely, 6.8% of individuals with airflow obstruction on spirometry were reclassified as not having COPD, and their outcomes resembled those without airflow obstruction, suggesting they may have been misclassified under older guidelines.
Findings from the CanCOLD cohort confirmed that individuals newly diagnosed using the new criteria also experienced significantly more exacerbations.
These results support the adoption of a multidimensional diagnostic model that goes beyond spirometry to better identify those at highest risk and improve clinical outcomes,” the authors wrote.
“Using the new COPD diagnostic schema, compared with individuals classified as not having COPD, those with a new diagnosis of COPD had greater all-cause and respiratory-specific mortality, more frequent exacerbations, and faster FEV1 decline,” they concluded.
“This new COPD diagnostic schema integrates multidimensional assessments to include additional individuals with high respiratory morbidity and to exclude individuals with airflow obstruction who do not have respiratory symptoms or evidence of structural lung disease.”